What I wish i'd known about NICU
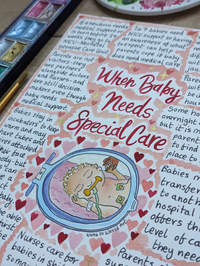
I used to think that special care was just for premature babies - but the majority of babies who receive neonatal care are actually born full term. 60% of babies in NICU are full term (after 37 weeks) and may need support due to infection, issues with breathing, feeding, jaundice or lack of oxygen to the brain.
Around 1 in 7 babies born in the UK are admitted to a neonatal unit. Having an awareness of what to expect and how to feel empowered would help parents cope and lessen their trauma if baby does need medical care, so I am urging antenatal teachers to include special care in their conversations with expectant parents - as 1 in 7 of those babies will need it.

Maggie's NICU story
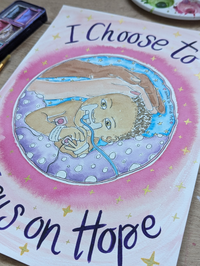
Until I became pregnant, I had the same conditioned view of birth as most women in the developed world (as a painful, terrifying, medical event) - and everything I learnt to the contrary was wonderful and enlightening and amazing. I felt so excited and blessed to be the kind of person who seeks to educate myself and challenge conditioned beliefs so that my baby could have the kind of beginning every child deserves.
But as it turned out, the Universe had other plans. After a healthy ‘low-risk’ pregnancy, labour started spontaneously during my 42nd week. After 36 hours of relentless back-to-back labour at home, there were concerns about her heart rate and we were transferred to hospital.

Maggie was in NICU for 10 days with Meconium Aspiration Syndrome after an emergency forceps birth. It was three days until we had confirmation from a doctor that she would definitely come home. Three days where we didn’t know if she’d live. It was three days until I could hold her, still attached to loads of wires. Five days until I could try to breastfeed her. I will always wonder if we’d asked to speak to a different doctor at first - a more sensitive and effective communicator - whether we’d have had better understanding and avoided those three days of terror, not knowing whether she would survive.
The hospital let us stay for five days on the maternity ward, and my husband wheeled me around. I could barely care for myself and my carefully-prepared postpartum plan with holistic rest and recovery went out the window. My wound from an episiotomy and 3rd degree tear became painfully infected, but when I was examined they said they couldn’t see any signs of infection. I persisted and it took three different courses of antibiotics before the infection eased and I was no longer in searing pain.

After the five days we had to travel back and forth to the hospital, but I refused to go home without her, so we stayed at my mothers. Leaving her there overnight, not being in the same building, was unbearable. It was like living in a nightmare.
On the outside I looked calm, but inside I was screaming, one long drawn-out anguished wail. I had to shut down in order to keep going, and in the process I now realise I had to shut her out too. I’ve done everything I can in the four years since to help us heal from the trauma, and since the day we brought her home we’ve never been apart - bedsharing, breastfeeding, babywearing and bonding with skin-to-skin.

Feeling powerless
A lot of the trauma I still carry is about her experience in NICU - knowing the fear and pain she would have felt and feeling powerless to help her. Looking back, I can see that not knowing straight away that we were ‘allowed’ to do certain things for her and with her added to our trauma. We felt helpless, shocked and totally disempowered as her parents.
If NICU had been discussed in our antenatal classes so i’d had an idea of what I could still do, and how I was still the parent and the one in charge, and what to expect - then it would have made the experience less traumatic for her and I. If we'd had someone to help guide and empower us whilst we were in NICU it would have made a difference to our experience. I needn’t have felt so helpless.

Not knowing how we could help
Not being told until two days in that our baby wouldn’t like the way we’d been stroking her gently, not being told straight away that I could have been using my expressed colostrum for mouth care to help seed her microbiome, not being told that we could bring in our own blankets for her incubator, not being told that I could have been the one washing her and changing her.
There’s many more. If the potential for NICU had been discussed in our birth education perhaps I could have known how to still feel empowered and like I was doing everything I could for her even though I couldn’t hold her or feed her.

As I was laying alone in the recovery area, surrounded by mothers and their babies, waiting for the epidural to wear off so I could be wheeled down to see my baby for the first time in a box - I took the initiative to start expressing colostrum myself as I knew it was crucial to do so as soon as possible after birth. I may not have got the birth and the golden hour or gentle postpartum period I wanted for us - so I was even more determined to make breastfeeding a success. I pumped religiously every two-three hours, including through the night, to establish my supply until she was ready to nurse. But when we tried she couldn’t latch, and we later had a tongue tie division.
Thankfully, nipple shields were suggested and they helped us to breastfeed for two months until we could finally nurse on our own. I feel so proud that I kept pushing to get the support we needed and managed to exclusively breastfeed her despite our difficult start, and went on to feed her until she was three.
What I want other NICU parents to know
What I wish I’d known when our full term baby needed special care after a healthy ‘low risk’ pregnancy, to help other parents in a similar situation know how to care for their NICU baby.
You can make a difference
There are ways you can reduce the stress and over-stimulation of the NICU environment for baby. Even if you can’t hold them, you can place still, resting hands at their head and feet to help them feel contained. This is better than soft, feathery stroking movements which may feel irritating and overstimulating.
You can minimise over-stimulation from noise, lights and smells, and improve baby’s environment in other ways such as:
partially-covering the incubator with a blanket
- allowing baby time to recover after tiring or stressful procedures
- warming hands and speaking before touching baby
- not wearing perfume or deodorant so baby can recognise your smell
- talking, reading and singing to your baby as much as you can to soothe them with familiar sounds
- providing comfort with breastfeeding or skin-to-skin during procedures if possible
- bringing in your own things to look after baby like nappies, hat, gloves and personalising your baby’s sleeping space with your own blankets and keepsakes
- helping to provide comfort to baby when you have to go by leaving them a soft toy or cloth which you’ve had against your skin.
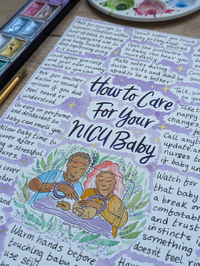
You are still their parent
In a scary situation it can be hard to remember, but it’s so important to know that parents are not visitors - they are partners alongside doctors and nurses - and are still the decision-makers even though baby needs medical support.
You can ask for another doctor or a second opinion if you don’t feel heard or understood. Make notes during doctor’s rounds, and don’t be afraid to ‘be a bother’ - ask as many questions - as many times - as you need to feel you are making informed decisions. Use B.R.A.I.N. (Benefits, Risks, Alternatives, Instinct, Nothing) to make empowered choices for your baby.
Know that you can call anytime you want an update on baby and trust your instincts if something doesn’t feel right.
You can take the lead
Don’t wait to be offered the opportunity to do things for your baby. Don’t assume that you can’t do something like hold them, clean them or change them because the nurses haven’t offered. Take charge of baby’s care, and be proactive (and pushy!) in asking for support so you can:
- have as much skin-to-skin as possible
- give kangaroo care in a sling or wrap
- understand your baby’s condition, needs, medications and treatments
- change nappies
- change bedding and remake the ‘nest’ to help baby feel contained
- give mouth and eye care with colostrum
express breastmilk regularly and establish breastfeeding
- manage tube feeding
- be there to support baby during procedures.